

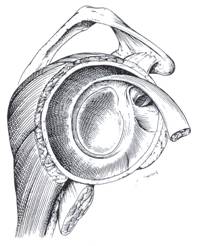
The shoulder joint is a ball and socket joint, with the humeral head (upper arm bone) as the ball and the glenoid as the socket. The glenoid (socket) is a shallow bone that is encircled with tissue called the labrum. (See Figure 1) The labrum acts as a stabilizer for the head of the humerus as it deepens the socket in which the humerus rests.
Instability can occur whenever the labrum is torn, stretched, or peeled back off the bone- which allows the head of the humerus to move away from the glenoid. This can occur after a shoulder dislocation, shoulder trauma, or as a result of repetitive motion. Some patients also have a genetic predisposition to develop shoulder instability.
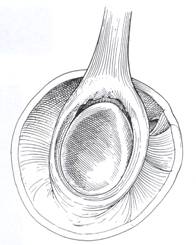
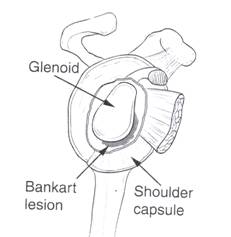
Instability can occur in one or multiple directions depending on where the labrum is damaged. Labral tears can be classified based on where the tears are located. If the superior or upper portion of the labrum is detached it is classified as a SLAP tear. (See Figure 2) If the lower labrum is separated from the bone it is classified as a Bankart tear. (See Figure 3)
Patients with shoulder instability can suffer from recurrent shoulder dislocations (complete popping out of the shoulder joint), recurrent subluxations (slipping in and out of the shoulder joint) or shoulder pain. Dislocations can cause fractures and rotator cuff tears. Osteoarthritis or wearing of the surface cartilage of the shoulder joint can also occur as a result of shoulder instability.
Once shoulder instability has occurred, occasionally further instability can be prevented with strengthening exercises. See Rehabilitation.
Patients may notice anterior, posterior or lateral shoulder pain with or without episodes of subluxation or dislocation.
Treatment involves both surgical and non-surgical options. If you have suffered a recent dislocation X-rays may be obtained to make sure the shoulder has returned to the correct position. An MRI may also be obtained to evaluate the labrum, shoulder joint and rotator cuff tendons.
1. Rotator cuff strengthening exercises strengthen the muscles and tendons surrounding the shoulder joint and act as secondary stabilizers. They also decrease inflammation in the rotator ruff tendons. These exercises can be done at home, at a gym or with a physical therapist. (See Rehabilitation)
2. Anti-inflammatory medications help decrease inflammation as well as treat pain.
3. Shoulder bracing can be effective for athletes who have recurrent shoulder dislocations.
Shoulder surgery is almost always done via arthroscopy (surgery guided by video imaging as opposed to open surgery), but in patients with recurrent instability open surgery may be recommended. Surgery stabilizes defects in the labrum, capsule and surrounding ligaments. Stabilization occurs with placement of a small anchor into the glenoid. Suture is attached to the anchor and used to secure the labrum, capsule, and ligaments to the glenoid.
Please watch the shoulder Surgical videos
Studies have shown that patients who have an unstable shoulder or who have dislocated their shoulder at a younger age are much more likely to continue to have problems with instability without surgical treatment. As the body ages tissue tightens. Therefore patients of an older age with instability are more likely to be successful with non-surgical treatment. However, older patients who dislocate are more likely to also do other damage to the shoulder such as tear the rotator cuff or fracture the humerus or glenoid.
Even in patients who require surgery we expect a return to all activities.