

There are several surgical options to treat knee osteoarthritis: (1) Arthroscopy; (2) Chondroplasty; (3) Microfracture / Abrasion; (4) Autograft OATS; (5)Allograft OATS; (6) Meniscus Reconstruction; (7) Tibial Valgus Osteotomy;
(8) Femoral Varus Osteotomy; (9) Autologous Chondrocyte Implantation; (10) Unicompartmental Arthroplasty; and (11) Total Knee Arthroplasty.
In addition to nonsurgical management of osteoarthritis, several surgical options exist. Surgical options include first a knee arthroscopy (scope) and chondroplasty. Chondroplasty is a smoothing of roughened articulate cartilage. The smoothing may decrease the friction inside the joint but is performed conservatively as to prevent thinning of the surface cartilage.

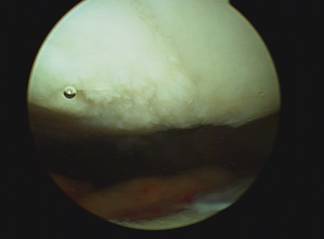
Abrasion arthroplasty, or micro-fracture, is appropriate for small areas of exposed bone or complete loss of cartilage. Abrasion of the area exposed bone is performed with a surgical pic which stimulates the bone to bleed allowing the bone to in response grow scar cartilage over the previously exposed area. The resulting cartilage growth and its effectiveness are variable between patients.
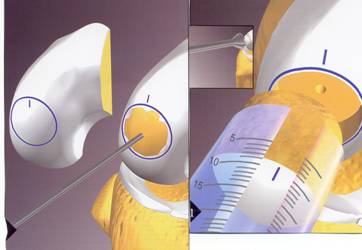
Osteochondral Autograft (or allograft) transplant (OATS procedure) can be performed for small to moderately large area of full thickness surface cartilage loss. These areas of full thickness cartilage loss are also referred to as grade IV chondromalacia. This procedure involves first removing a cylinder shaped dowel of bone which is lacking surface cartilage and replacing it with a dowel or cylinder of bone with intact surface or articulate cartilage. Both dowels are the same size so when they are switched there is a press fit and no hardware is needed to secure it in place.
The replacement dowel of bone with surface cartilage can either come from a non weight bearing area of bone and surface cartilage from your knee (AUTOGRAFT) or from a cadaver (ALLOGRAFT). If the lesion or area lacking surface cartilage is less than 20mm an autograft OATS may be performed, using either one or a few bone and cartilage plugs. If the lesion to be resurfaced is larger than 20mm, taking tissue from a cadaver or an allograft is needed. This tissue must be ordered and this may require a second surgery. The size of the lesion and appropriateness of either procedure is usually not known until the arthroscopy is performed.
Rehabilitation after an OATS procedure includes using crutches and partial weight bearing activity only for 3- 6 weeks, depending on the size of the lesion.







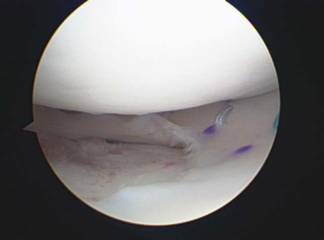
A meniscal transplant involves implanting either a medial or lateral meniscus from a cadaver into a knee joint that is lacking greater than 50% of meniscal cartilage. X-rays or an MRI are used to measure the patient's knee to determine the dimensions of the meniscus needing to be ordered. The wait for a meniscus may be a few weeks to several months. This procedure however, has only been found to be useful in patients with intact surface cartilage above and below the meniscus. Thousands of meniscal transplants have been done world-wide; Dr. King has done hundreds.
Rehabilitation after this procedure includes walking with crutches and a knee brace for the first 3-6 weeks with physical therapy usually starting the first or second week after surgery.

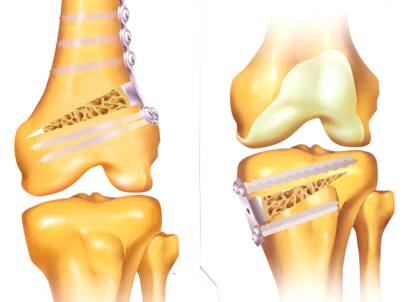
Often patients with knee osteoarthritis may have more arthritis on either the inside (medial) or outside (lateral) of the knee, causing the alignment of the knee joint to shift towards becoming bow-legged or knock-knee. Unfortunately once alignment is no longer even activity and pressure on the knee joint can cause an acceleration of wearing of the vulnerable side of the knee as more and more weight is now transferred onto that area. An Osteotomy is a realignment procedure that unloads the vulnerable or arthritic side of the knee and puts the majority of the load of the knee joint onto the underutilized cartilage on the other side of the knee.
An Osteotomy is performed by wedging open either the tibia (shin bone) or femur (thigh bone) and adding bone graft putty to create new bone growth into the wedged area. After this procedure patients are on a home motion machine then progress to physical therapy, while using a brace and crutches for the first 4-6 weeks after surgery until the bone is well healed. This procedure is very successful in relieving symptoms and preventing or delaying an artificial knee in many patients.

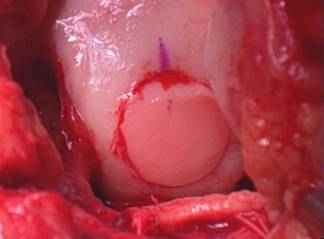
Autologous Chondrocyte Implantation or Carticel is a procedure that first requires a knee arthroscopy where a biopsy of your cartilage cells is obtained and then shipped to a laboratory where these cells are used to produce more cartilage cells. Six weeks after the biopsy these cells are reimplanted into your knee over the cartilage defect. A fibrous sleeve is used to hold the cells over the defect. These cells have been shown to grow and result in new cartilage matrix.
The first disadvantage to this procedure is that is requires two procedures, the second of which is an open procedure The second disadvantage is that some reports note that the new cartilage is not significantly different from the new cartilage found after an abrasion or microfracture procedure (please see above).
Another option for patients with osteoarthritis in one area of the knee- usually medial or lateral is an artificial resurfacing of the cartilage surface, called a unicompartmental knee replacement. This procedure is successful in relieving symptoms from osteoarthritis if the arthritis is limited to one compartment or area of the knee.
Artificial joint resurfacing involves caping the end of the femur (thigh bone) and tibia (shin bone) with plastic and or metal pieces. These pieces are glued in place to form an artificial joint surface.
This procedure can be very effective in eliminating painful and severe OA, but it is limited by the fact that the articular components (plastic and metal) will eventually wear out and need to be replaced. Inactive people early loosening of the components can occur. For these reasons most orthopedic surgeons try to delay artificial resurfacing procedures until late in life. Biologic living joints can live 60-80 years. No artificial joint can do this.