

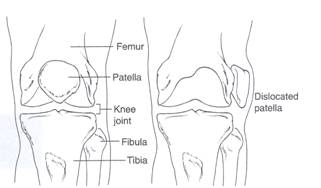
Patellar Instability can be seen with dislocation, subluxation or maltracking. Acute dislocation is a traumatic event when the knee cap slips laterally and locks out of place. Usually this results in a trip to the ER where it is put back into place. Subluxation of the knee cap is when the bone slips in and out of place but does not lock out. Maltracking is when the knee cap is not in the correct anatomical alignment causing increased wearing of one side of the knee cap.
Some patients have a shallow trochlear groove which allows the knee cap to slide out of position easily. Other patients have flexible tissue that can predispose them to patellar instability. Weak quadriceps muscles can also result in a knee cap that is not tracking correctly.
Maintaining quadriceps strength can prevent patellar femoral many problems, however, it does not always prevent instability. A knee patellar stabilization knee brace may also be helpful in preventing instability.
Patients may have acute dislocation or subluxation episodes or they may present with anterior knee pain.
After an acute episode, the patient may be initially treated with a brace and crutches, and possibly X-rays or an MRI. X-rays are useful to determine that the patella is back in the correct position. An MRI is useful to evaluate damage to the surrounding tissues and surface cartilage as a result from the chronic condition or acute event. Based on examination, history, and radiology studies benefits of surgical and non-surgical treatment can be determined.
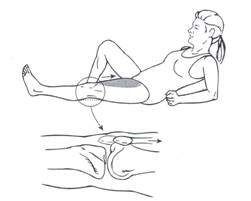
Nonsurgical treatment focuses on strengthening of the quadriceps muscles. Strengthening is key is preventing further dislocation or subluxation episodes, as the quadriceps act to pull the knee cap medially. Rehabilitation can be started with a physical therapist but the patient must be prepared to continue the exercises most days of the week at home or at the gym.
Knee braces with a patellar buttress or taping may also help. For patients with knee pain from increased wearing or early osteoarthritis of the surface cartilage behind the knee cap viscosupplementation injections can be used. Viscosupplementation injection or lubrication injections help about 50% of patients. They increase and supplement the viscosity of the natural joint fluid allowing for a decrease in symptoms and increased tolerance of strengthening exercises.
Injection are once a week for three weeks
Surgical treatment choices for patellar instability include a knee arthroscopy, proximal patellar realignment, and distal patellar realignment. A knee arthroscopy or "scope" could smooth rough surface cartilage or remove loose bodies.
A proximal patellar realignment involves tightening the tissues on the medial (inside) of the knee cap and releasing the tissues on the lateral (outside) of the knee cap. This help the knee cap track correctly and prevents it from sliding out of position.
Distal patellar realignment involves shifting the bony insertion of the patellar tendon medially (inward) on the tibia or shin bone. This adds further support to keeping the knee cap shifted inward and in correct anatomical alignment.
It is important to remember that with any surgical intervention strengthening after the surgery plays an important role in the success of the procedure.
Prognosis after an episode of patellar instability is largely age dependant. Patients who are in their teens or twenties who dislocate are highly likely to have further instability episodes and less likely to successfully rehabilitate with exercise alone, and may require surgical stabilization. Individuals who are forty or older are much more likely to successfully return to all activities with exercise alone.
All exercises should not cause increased pain or swelling. Work up to at least 3 sets of 20 repetitions, at least 4 days a week. See Fig 2-7.




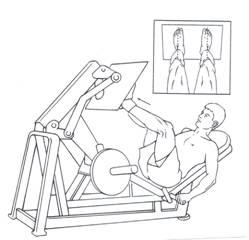
Stationary bike and elliptical are also recommended.